Alaska Department of Health and Social Services Weekly Case Analysis
October 4-10, 2020
Case trends and predictions
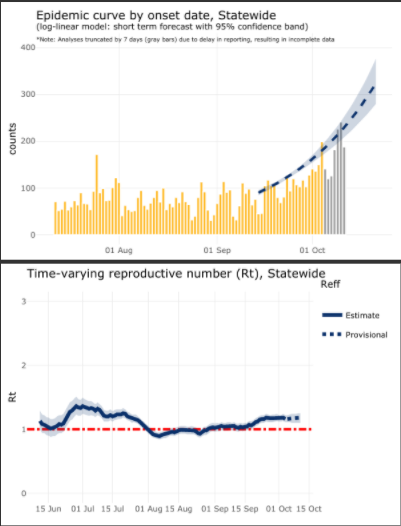
- More cases (1,256) were reported in Alaskans this week than any previous week, beating last week’s record number of new cases (891) by more than 40%. Alaska continues to see a sharp acceleration in new cases.
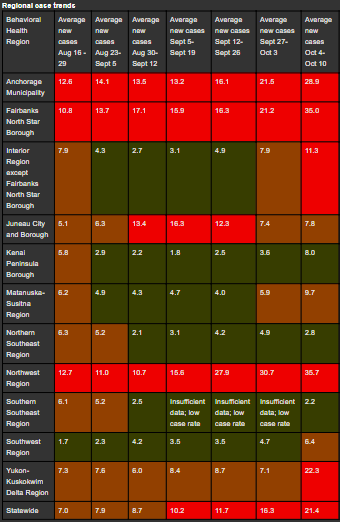
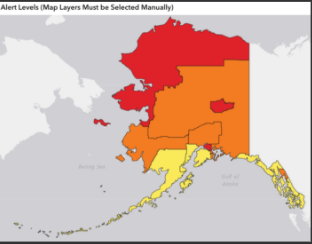
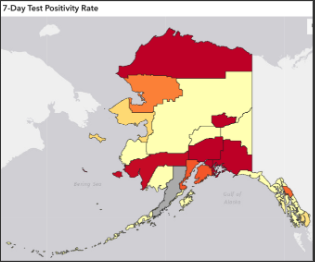
- The sharp acceleration affected urban and rural regions. The largest increases in case rates were in the Yukon-Kuskokwim Delta Region, Anchorage Municipality and Fairbanks North Star Borough. The Northwest Region continues to have the highest two-week average case rate of any region of the state and saw increases this week.
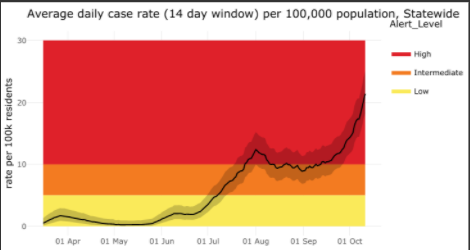
- The daily state case rate as of October 10 data is 21.4, up from 16.3 on October 3, a 31% increase. This number is cases per 100,000 people averaged over the last 14 days. The state alert level is high.
- Compared to other states’ case rates, Alaska’s average case rate per capita over the last 7 days (25.5 average daily cases over the last week per 100,000) remains at the thirteenth highest of US states, just below Wyoming (27.3) and worse off than Missouri (24.4). If Anchorage were its own state, its 7-day case rate (34) would put it at rank #6, between Utah and Idaho, and if Fairbanks were a state, its 7-day rate of 40.7 would make it #5 in the nation, just behind Wisconsin. The Bethel Census Area would be #4 with a 7-day rate of 49, while the Northwest Arctic Borough’s 7-day case rate of 75 puts it at a higher average case rate this week than any state average in the US. Nationally, cases have been rising since mid-September, and increases have been seen in most states this week. 26 states currently have 7-day average case rates over 15 per 100,000 and an additional 17 states saw increases in their 7-day average case rate this week.
- The reproductive number, a measure of contagion, is currently estimated to be approximately 1.18, a significant increase from 1.03 two weeks ago. A reproductive number of 1 means that each person who is diagnosed with COVID-19 gives it on average to one other person, so this increase means that Alaskans with COVID-19 are spreading it more readily than they were two weeks ago. A reproductive number of more than 1 also means that the epidemic is growing, and the goal is to have enough people wear masks, stay at least 6 feet from others, and stay home and get tested when they are sick that Alaska’s reproductive number decreases to well below 1. Our reproductive number was below 1 as recently as late August.
- An updated model epidemic curve predicts Alaska’s cases will continue to accelerate over the next week. Two weeks ago, cases were now expected to double every 105 days, with a daily projected growth rate of 0.66%. This projection has worsened, with cases now expected to double around every 20 days and a daily projected growth rate of around 3.5%.
- Nonresident cases, which peaked in late July, decreased over August and until this week had remained at an average of around 3 new nonresident cases per day; this week around 5 new nonresident cases were identified per day.
- Alaska continues to have the fewest COVID-19 related deaths per capita of any US state, but now has more total deaths than both Vermont and Wyoming.
Regional trends
- Anchorage Municipality, Fairbanks North Star Borough, the Northwest Region and the Y-K Delta Region all had substantial and concerning increases in case rates this week, indicating accelerating cases and high levels of community transmission. The largest acceleration seen was in the Y-K Delta Region, with the two-week average case rate more than tripling, from 7.1 to 22.3. Fairbanks North Star Borough saw a 65% increase in case rate, from 21.2 to 35.0, while Anchorage Municipality’s case rate increased by 34% to 28.9 from 21.5 last week.
- Northwest Region increased by 16% from 30.7 to 35.7, remaining the highest rate of new cases of any borough reported.
- The Interior Region moved into the high alert level this week with an increase to 11.3 from 7.9.
- Mat-Su saw another significant case increase this week and is nearing the high alert level, with a case rate of 9.7 from 5.9 last week.
- The Southwest region entered the intermediate alert level with a rise from 4.7 to 6.4.
- Juneau City and Borough remains in the intermediate alert level with a modest increase this week from 7.4 to 7.8.
- The Interior Region, Kenai and Northern Southeast Region also saw increases this week but remain at the low alert level.
New cases, hospitalizations and deaths
How COVID-19 spreads in Alaska
- The week of October 4-10 saw 1,256 new cases in Alaskans, a 41% increase from the week of September 27 -October 3’s 891 new cases, for a total of 9,686 cumulative cases in Alaskans.
- This is the highest number of new cases in one week ever reported in Alaska. The previous week, Sept 27- Oct 3, was the second highest. The third highest was 740 cases, reported between July 26 and August 1.
- Cumulative hospitalizations increased to 324 with 24 new this week.
- Deaths among Alaska residents increased by 2 to 60 total.
- There were 36 nonresident cases identified this week, for a total of 1001.
How COVID-19 spreads in Alaska
- Most new infections among Alaskans are from community spread, not from travel. Most Alaskans get the virus from someone they work, socialize, or go to school with.
- Many cases do not have a clear source, meaning that contact tracers have not been able to identify where the person got the virus. This means that there are cases in our communities that we do not know about.
- Many Alaskans who are diagnosed with COVID-19 report that they went to social gatherings, community events, church services and other social venues while they were contagious but before they knew they had the virus.
- The distribution of cases among people of different races and ethnicities has not changed significantly since last week.
- Cases continue to increase most rapidly in young adult Alaskans, especially those aged 20-29, and among Alaskans 10-19 and 30-39.
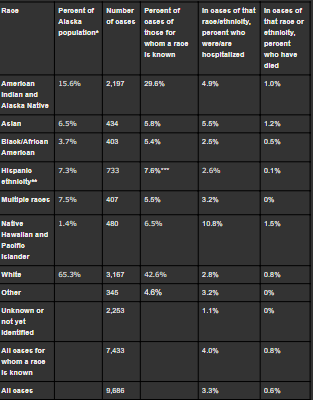
Distribution of cases compared to population distribution and distribution of cases, hospitalizations and deaths by race and ethnicity
Includes data from all cases reporting one or more races. Based on these data, American Indian and Alaska Native as well as Native Hawaiian and Pacific Islander populations are disproportionately affected. One factor limiting interpretation is that a greater proportion of tests from the Alaska Native Tribal Health system currently have race indicated than tests from other sources, which may mean that cases in Alaska Native People are more likely to be reported as such than cases in people who receive care through non-tribal health systems. However, this should not significantly impact Native Hawaiian and Pacific Islander population case counts.
If race or ethnicity is not identified with the initial test, contact tracers will attempt to collect this information, but these data are often delayed resulting in many cases still labeled under investigation or unknown. Additionally, people who are hospitalized or have died with COVID-19 are more likely to have a race identified. Because many cases that previously had unknown race or ethnicity now have an identified race or ethnicity, numbers of cases in different race and ethnicity categories have increased since last week beyond the number of new cases, so these numbers affect both newly diagnosed and newly categorized but previously counted cases.
Includes data from all cases reporting one or more races. Based on these data, American Indian and Alaska Native as well as Native Hawaiian and Pacific Islander populations are disproportionately affected. One factor limiting interpretation is that a greater proportion of tests from the Alaska Native Tribal Health system currently have race indicated than tests from other sources, which may mean that cases in Alaska Native People are more likely to be reported as such than cases in people who receive care through non-tribal health systems. However, this should not significantly impact Native Hawaiian and Pacific Islander population case counts.
If race or ethnicity is not identified with the initial test, contact tracers will attempt to collect this information, but these data are often delayed resulting in many cases still labeled under investigation or unknown. Additionally, people who are hospitalized or have died with COVID-19 are more likely to have a race identified. Because many cases that previously had unknown race or ethnicity now have an identified race or ethnicity, numbers of cases in different race and ethnicity categories have increased since last week beyond the number of new cases, so these numbers affect both newly diagnosed and newly categorized but previously counted cases.
*Based on US Census Bureau 2019 estimates: https://www.census.gov/quickfacts/AK
**By federal convention, ethnicity is not mutually exclusive of race, so cases identifying Hispanic ethnicity are also counted under a race category.
***Reports the percent of cases of those for whom an ethnicity is known.
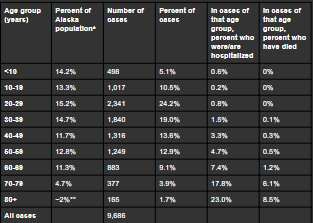
Distribution of cases compared to population distribution and distribution of cases, hospitalizations and deaths by age group
Includes data from all cases. For all ages, the percent of cases in that age group who have been hospitalized or who are deceased is either the same or decreased from last week. Hospitalizations and deaths tend to lag new cases by several weeks, so we expect to see case numbers rise (and percentages therefore fall) well before we see substantial increases in hospitalizations or deaths.
**By federal convention, ethnicity is not mutually exclusive of race, so cases identifying Hispanic ethnicity are also counted under a race category.
***Reports the percent of cases of those for whom an ethnicity is known.
Distribution of cases compared to population distribution and distribution of cases, hospitalizations and deaths by age group
Includes data from all cases. For all ages, the percent of cases in that age group who have been hospitalized or who are deceased is either the same or decreased from last week. Hospitalizations and deaths tend to lag new cases by several weeks, so we expect to see case numbers rise (and percentages therefore fall) well before we see substantial increases in hospitalizations or deaths.
*Based on US Census Bureau 2019 estimates via Census Reporter: https://censusreporter.org/profiles/04000US02-alaska/
**Margin of error is at least 10% of the total value
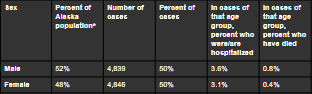
Distribution of cases compared to population distribution and distribution of cases, hospitalizations and deaths by sex
**Margin of error is at least 10% of the total value
Distribution of cases compared to population distribution and distribution of cases, hospitalizations and deaths by sex
*Based on US Census Bureau 2019 estimates via Census Reporter: https://censusreporter.org/profiles/04000US02-alaska/
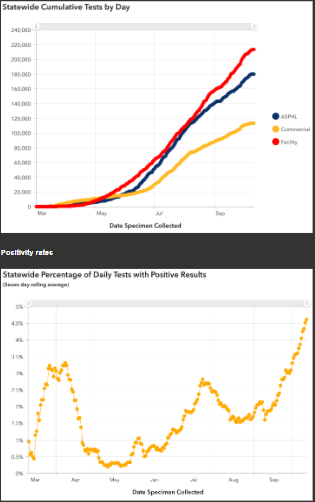
Testing trends
Testing trends
- Testing increased at a steady rate throughout May, June and July, slowed in mid-August, and is starting to increase again. Over half a million tests have been performed so far in Alaska (505,924) and current laboratory turnaround times average 1-2 days.
- Alaska has the capacity to continue expanding testing. DHSS can assist in materials for setting up new testing sites and is pursuing all avenues for expanding testing.
- The statewide test positivity rate went from 3.9% to 4.6% this week, which is the second week in a row that it is the highest it has ever been. Positivity rate is calculated by dividing the number of positive tests by the total number of tests performed over a given period of time, averaged over the past seven days. Statewide test positivity had not been above 3% since April, and had never before exceeded 3.5%, but has been climbing from below 2% in early September and the increase has accelerated.
- Currently, the national average is 5.0%. While many states have a higher positivity rate than Alaska does, this rise is concerning because the positivity rate is our best measure of whether our testing capacity can keep up with current cases. A rise in positivity rate reflects that testing is not increasing as fast as the current increase in cases. Since Alaska’s per-capita testing capacity is more robust than almost any other state, the finding that the positivity rate is nearing the national average is concerning. Source: Johns Hopkins
- The reported test positivity rate is currently highest in the Fairbanks North Star Borough, with a rate of 11.8%, increased from 10.5% last week. Anchorage Municipality has a test positivity rate of 5.0%, an increase from 4.6%; similarly the Mat-Su Borough, Bethel Census Area and Valdez-Cordova Census Area have rates around 5%. The North Slope Borough’s reported test positivity rate is now 6.25%, significantly improved from that reported last week (19.2%), although is limited by being based on a smaller number of tests. The Northwest Arctic Borough’s positivity rate is reported as 2.7%, much better than last week’s rate of 6.4%.
- Test positivity is a good measure of whether testing is adequate in a given area, since it is affected by the number of tests performed as well as the number of new cases in an area. However, because it depends so much on the number of tests performed, it tells us more about whether we are doing enough testing than about how much virus is spreading in a community. It cannot be used to compare the amount of virus spread in one state to another, but it can be used to compare whether different states are doing adequate enough testing to be able to measure their case rate. It is also affected by any delays in reporting, since positive tests are sometimes reported faster than negative tests. A case rate can give good information about how much virus is spreading in a community, as long as the test positivity is low, so these measures can work together to help us understand the spread of virus in a community. A community test positivity rate under 5% is currently generally accepted as being low enough to estimate that a community’s case rate is reasonably accurate.
- In late August, Alaska led the nation in most tests per capita and continues to be among the top 3 states in tests per capita. Alaska’s high testing rates likely affect our hospitalization and death rates, since in places where tests are restricted to people who are very ill, many asymptomatic or mildly symptomatic COVID-19 cases are missed. In Alaska, testing is somewhat more available in many communities than in many communities in the lower 48, so we may detect more COVID-19 cases relative to the real number of people with COVID-19 than in states that do less testing per capita. Hospitalization and death rates are calculated by dividing the number of people who were hospitalized or who died by the number of people in that group that were known to have COVID-19, regardless of the severity of their illness.
- We do not have a reason to believe that the strains of COVID-19 are any less virulent in Alaska than elsewhere; in fact, in the genetic studies done so far of COVID-19 strains circulating in Alaska, virus that was as virulent or more so than that circulating in the Western United States was identified. This means that the virus present in many communities in Alaska has the ability to make people of all ages very sick if it is allowed to continue to spread.
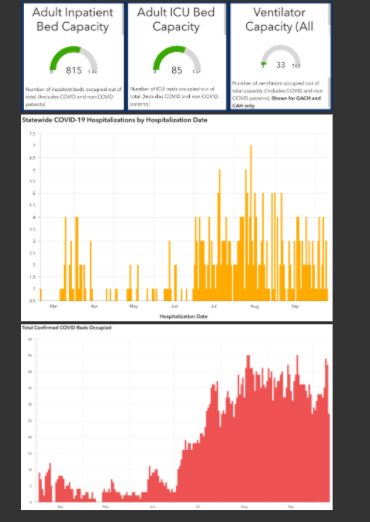
Health care capacity
- The data hub has been updated to reflect adult and ICU hospital bed capacity around the state. Adult bed occupancy can also be viewed at the following link which appears at the top of the data hub page: https://coronavirus-response-alaska-dhss.hub.arcgis.com/datasets/table-6c-geographic-distribution-of-adult-hospital-survey-results/data
- Hospital data includes inpatient beds and ventilators located all around the state, including some in smaller hospitals without ICU capacity. Hospital beds also do not necessarily represent staffed beds, as staffing can change quickly, particularly if a community has many health workers impacted by COVID-19.
- Currently, 36 Alaskans with suspected or confirmed COVID-19 are hospitalized. Of these, 8 are currently requiring a mechanical ventilator.
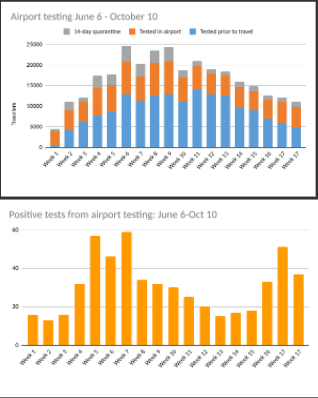
COVID-19 and travel
- Travel is not currently thought to be a main factor in most new COVID-19 infections in Alaska, meaning that most Alaskans who get COVID-19 are getting it from social, work or family contacts rather than travel. New cases in nonresidents have diminished since summer peaks, averaging around five new cases per day over the last week, up from around three per day the previous few weeks.
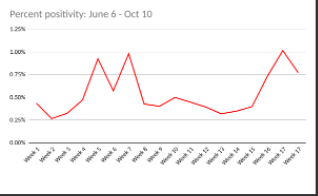
- Testing in airports is now in its 18th week, with 327,725 passengers screened total, 12,712 in the past week. In the last week, 4,911 (39%) of travelers tested prior to travel, 4,800 (38%) tested in the airport, 1,388 (11%) selected a 14-day quarantine and 1,613 (13%) followed another workplace and community protection plan. Of those tested in AK airports, 37 have been reported as positive, for a 0.8% positivity rate. Since airport testing began, 164,204 (50%) of travelers have tested prior to travel, 101,692 (31%) have been tested in an airport in Alaska, 33,469 (10%) have selected a 14-day quarantine, and there have been 551 positive tests overall. This does not include anyone who tested positive later in their travel quarantine or isolation period, only those who tested positive at time of entry.
- The positivity rate in airport tests has been significantly higher than average in the past three weeks, averaging 0.84% compared to an overall average of 0.54%. As expected, the airport test positivity rate continues to be much lower than the state's average positivity rate as these tests are performed in people who believe themselves to be well enough to travel, and many travelers to Alaska test before they arrive in Alaska, meaning that many infections are likely caught before a traveler arrives.
What Alaskans should do
Further information
- Anyone with even one new symptom of COVID-19 (fever, chills, cough, shortness of breath, difficulty breathing, fatigue, muscle aches, body aches, headache, new loss of taste or smell, sore throat, congestion, runny nose, nausea, vomiting, or diarrhea), even if it is very mild, should get tested for COVID-19 right away and immediately isolate themselves from others by staying home, staying away from others, and not leaving their house except to seek testing or other medical care. Tests are most accurate in the first few days of symptoms, so testing as soon as possible after the first symptom starts is important, even if the symptom is very mild. Getting tested right away also helps contact tracers move as quickly as possible.
- Alaskans can help contact tracers work to slow the spread of COVID-19 by answering the phone promptly and providing accurate information.
- Alaskans should avoid gatherings, wear masks when around any non-household member, keep six feet of distance from anyone not in their household and wash hands frequently to slow community transmission of COVID-19.
Further information
- The Frequently Asked Questions webpage at https://covid19.alaska.gov/faq/ is often the quickest route to an answer regarding testing, travel, health mandates and other COVID-19 information.
- Please see the State of Alaska COVID-19 information page at http://dhss.alaska.gov/dph/Epi/id/Pages/COVID-19/default.aspx for more information about the virus and how individuals and businesses can protect themselves and others from transmission.
- For the most up-to-date case information, see the Alaska Coronavirus Response Hub dashboard: https://coronavirus-response-alaska-dhss.hub.arcgis.com/. Some data may change as more information comes to light through contact tracing and other public health work.
- For questions regarding DHSS COVID response, including mandates and alerts, email [email protected].
Are you looking for a shipping solution? Maybe you need to change freight carriers? Find out what the hard working and reliable people at Team Worldwide can do over land, sea and air